Bringing new life into the world is a miraculous journey, but for some mothers, the path becomes fraught with challenges. Taylor McKey can attest to this as she faced a life-threatening condition called placenta percreta during her second pregnancy.
Placenta percreta is the most serious form of placenta accreta, where the placenta abnormally attaches too deeply into the uterine wall. Unlike a typical pregnancy where the placenta detaches easily after childbirth, in percreta, it can penetrate the uterine muscle and even reach adjacent organs. This abnormal attachment poses significant risks, especially during delivery, as it increases the likelihood of severe bleeding and complications.
Although placenta accreta is considered rare, one in 2,500 pregnancies, maternal mortality occurs in one in 272 births. Women with a history of C-sections are more at risk for developing placenta accreta, and the risk for women with two or more C-sections is as high as 40%.
“Diagnosis is challenging, especially when it’s a subtle case,” said Sarah Shepard, D.O., a maternal-fetal medicine specialist with Obstetrix® of Colorado, part of Pediatrix® Medical Group. “Undiagnosed is when you’ll have the greatest blood loss. There’s a 7% mortality with placenta accreta spectrum disorder, so when moms with the condition deliver and there’s not adequate blood supply and where they don’t have surgeons who are well versed in caring for women with placenta accreta, that is when they can have more complications and even die from a hemorrhage.”

Taylor’s Diagnosis and Pre-Delivery
Taylor, a pediatric nurse practitioner from the small town of Eagle, Colorado, was 20 weeks pregnant when she had an ultrasound as part of her routine prenatal care. The ultrasound, which was performed by Obstetrix of Colorado, revealed possible placenta accreta. At 30 weeks, the ultrasound was repeated, which further suggested she had the condition. At 31 weeks, an MRI was performed, verifying the diagnosis, and Taylor was advised to relocate to Denver within 20 minutes of Presbyterian/St. Luke’s Medical Center for the remainder of her pregnancy.
“We use a team approach through our placenta accreta program at Presbyterian/St. Luke’s Medical Center, working closely with the western slope and other physicians in Wyoming, Nebraska and throughout the Denver area,” said Dr. Shepard. “If we feel there is a high risk for there to be an invasive placenta, then we have our patients stay near the hospital temporarily so they can deliver their babies in Denver with our experienced accreta team.”
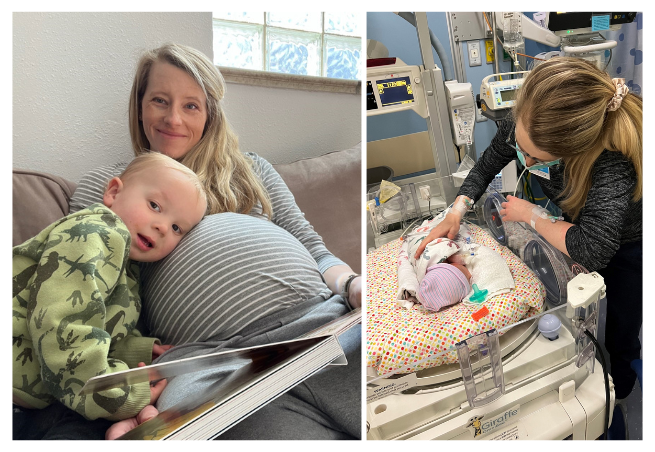
Taylor and her husband, along with their toddler son and family dog, rented a house close to the hospital. Together with Dr. Shepard and the hospital’s placenta accreta team, a plan was developed and Taylor would deliver by cesarean section at 35 weeks’ gestation.
“Everything was moving so fast, and it was very stressful and scary,” said Taylor. “We needed to be near the hospital in case I went into labor before the scheduled delivery date. So, we had a ‘crash plan’ in place for the unexpected. I knew little about placenta accreta, Presbyterian/St. Luke’s Medical Center or Obstetrix of Colorado. I didn’t know my care team, and I didn’t know until my formal diagnosis that the hospital had a placenta accreta program. I had to take a leap of faith with everything and had little time to process what was actually happening.”
During all the chaos of learning about her diagnosis and relocating her family to Denver, Taylor also learned that in addition to having a C-section delivery, she would need a hysterectomy at the same time. While the news was devastating, she could only focus on a safe delivery for her and her baby. The fallout of anything else would come later.
“With Taylor’s diagnosis, a C-section followed by a hysterectomy is the standard of care,” said Dr. Shepard. “When we entered into the abdomen, we could see that it was a true percreta, and there was no way to avoid a hysterectomy. She required four blood transfusions after delivery, which is typical and why it is crucial for moms like Taylor to be in a facility that specializes in these types of complex pregnancies and deliveries.”
A C-Section, Hysterectomy and Baby George
On Feb. 10, 2023, Taylor was taken to the operating room where her multidisciplinary team was waiting to perform two major surgeries — a C-section followed by a hysterectomy.
“One of the scariest moments in the hospital was when I was wheeled into the OR with a cooler of blood at the end of my bed,” said Taylor. “It was very daunting.”
Because of the complexity of placenta percreta, the two procedures took several hours. When baby George was safely delivered, Dr. Shepard and the team successfully completed a hysterectomy.
“Dr. Shepard has this amazing calming presence,” said Taylor. “She definitely put me at ease. She had a lot of confidence in her abilities and her knowledge of the diagnosis. She answered my questions thoroughly and gave us the confidence that she’s who we wanted to do the delivery.”
Being born five weeks early, George was taken to the neonatal intensive care unit (NICU), where he stayed for a week getting specialized care from the NICU team. Taylor was discharged from the hospital after four days.
“We were able to take George home with some oxygen because of our high altitude,” said Taylor. “But other than that, he was just fine and healthy.”
It would take Taylor several months to physically recover from her major surgeries. Emotionally, it would take longer.

The Fallout
While Taylor and George where both well and back at home, the type of trauma Taylor experienced leading up to, during and after delivery would take a toll. Learning she had a potentially life-threatening complication was shocking. Having to leave her home and job to be near the hospital was stressful. Getting the news that a hysterectomy was necessary was devastating. Going through six hours of surgery was traumatic.
And if that wasn’t enough, at four weeks old, George got respiratory syncytial virus (RSV) and had to be transported back to Denver for another week in the NICU.
“I think those two things back-to-back — the C-section with hysterectomy and George getting ill — caused some serious trauma,” Taylor said. “I was starting to not feel safe where we lived because we didn’t have access to the medical care we needed. I was having serious anxiety and started having nightmares and flashbacks of being on the OR table and of when George got sick at home and stopped breathing. So I reached out to Jen Adams, a counselor on the accreta team, and asked for a recommendation for counseling. I worked with a trauma therapist every two weeks for about six months who specializes in birth trauma, and she really helped me work through a lot of those things.”
While Taylor had never dealt with anxiety, everything she had gone through began mounting. She and her husband weren’t sure if they were finished having kids or if they were going to try for another, so they were mourning the loss of the decision being taken from them. Even going to the place near her work where she took the call being told she needed to relocate to Denver and have an early delivery triggered a lot of emotions.
“It's so important to address those things in the moment before they become bigger, more engrained problems in the future,” she said. “Even women with a normal pregnancy and delivery can experience postpartum depression and anxiety, but to have a traumatic birth puts you more at risk for sure. It was vital for me to get the help I needed afterward to be able to process everything I had gone through in a healthy way.”
 Prenatal Care Saved the Day
Prenatal Care Saved the Day
Taylor cites prenatal care as the saving grace in her situation and encourages all pregnant women to follow their doctor’s prenatal recommendations.
“Without ultrasounds, I would have had no idea that I had a life-threatening condition,” she said. “I felt great during my pregnancy. I had no signs of bleeding or pain. There’s no way I would have known, and my situation would have been vastly different had it not been found on an ultrasound.”
For Taylor, early detection, comprehensive prenatal care and a supportive health care team made a substantial difference in ensuring the safety and well-being of her and baby George.