When North Texas mom Liberty Riggs was pregnant with her third child, Seamus, she learned he had two rare congenital anomalies — duodenal atresia, an intestinal obstruction and Tetralogy of Fallot with severe pulmonic valve stenosis, a heart defect. Given the high-risk nature of her pregnancy, she was enrolled in Medical City Healthcare's Maternal Fetal Institute, which provided the opportunity to consult with specialists prenatally and plan for Seamus’s care once he was born.
That’s when Liberty and husband Joshua met James Davis, M.D., pediatric surgeon at Pediatrix® Surgical Associates, and the neonatal intensive care team at Pediatrix® Neonatology of Texas, led by Clair Schwendeman, M.D.
“Duodenal obstruction can take multiple forms,” said Dr. Davis. “My job is basically to give an overview of what happens soup to nuts in a general way, from what and how this could be, the pathology of it and talking them through what will happen immediately after birth. We talked about the different ways it might be managed depending on how severe the cardiac issues were.”
The care team laid out a road map of what would happen after Seamus was born. The neonatal team would attend Liberty’s delivery and stabilize Seamus, and Dr. Davis would await clearance from the cardiology team before moving forward with the intestinal repair.
On Nov. 3, 2022, Seamus was born at 37 weeks at Medical City Dallas. It was then that a surprise finding was discovered — a third birth defect, tracheoesophageal fistula (TEF), an abnormal connection between the esophagus and the trachea, which would increase Seamus’s risk and the complexity of his surgeries.
A Shift in the Care Plan
Early diagnosis and surgical intervention of the duodenal atresia and TEF were crucial to ensuring Seamus could successfully feed.
As Dr. Davis and team prepared for the duodenal obstruction repair, an unsuccessful attempt at passing a decompression tube indicated that something else was amiss.
“Through the workup and imaging, it became apparent that he also had a TEF,” said Dr. Davis. “This is a fancy way of saying that the esophagus is not completely in continuity from the mouth all the way down to the stomach.”
While that in and of itself is a significantly concerning condition, it’s that much more concerning if there’s no way for oxygen to pass through the intestine, which was the case due to the duodenal obstruction. Seamus was already facing reduced oxygen reserve because of his heart defect. Additionally, the team discovered that his aorta branched off on the opposite side of where it normally comes off, further complicating the repair.
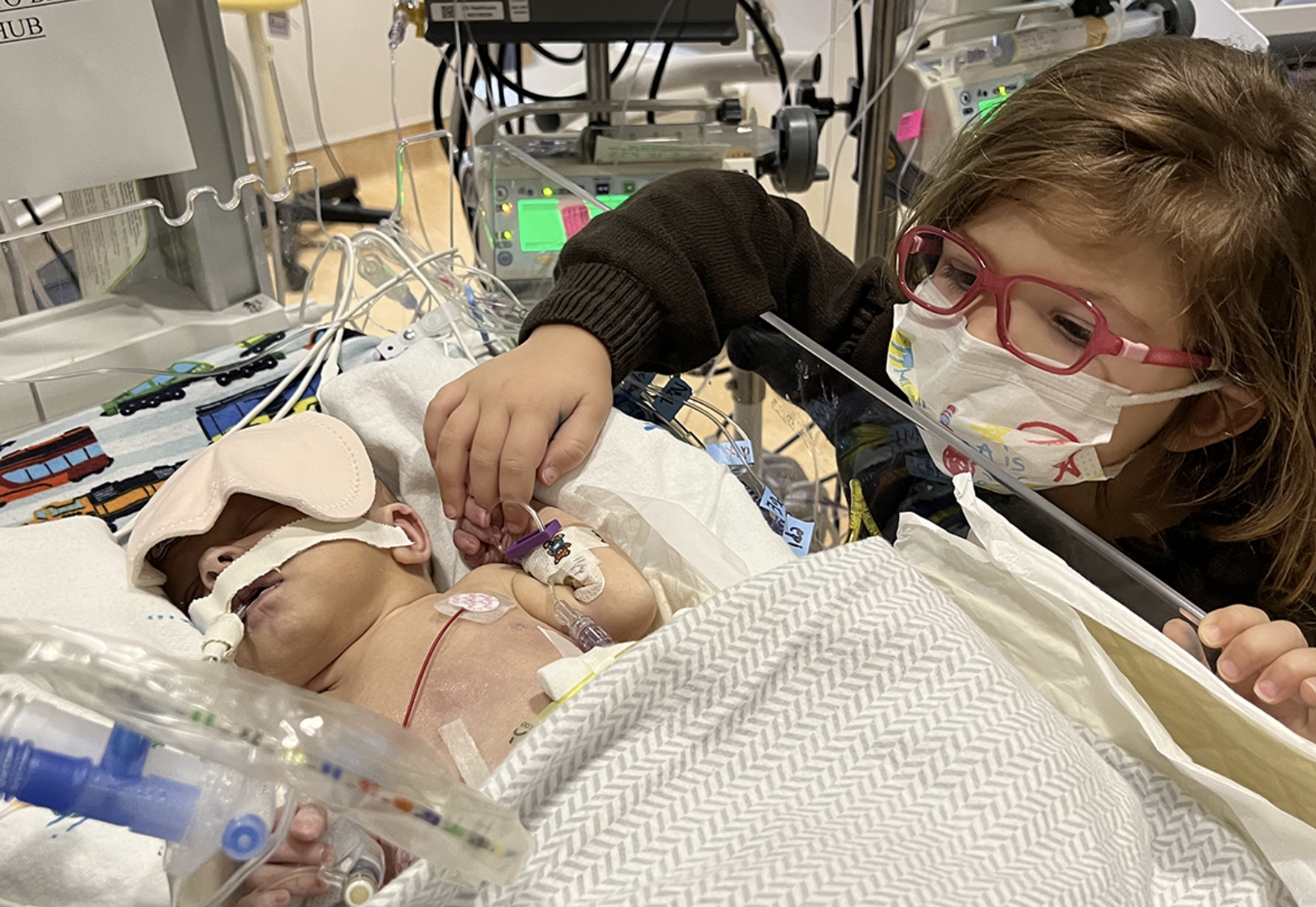
Following close overnight monitoring in the neonatal intensive care unit (NICU) and consultation with the cardiologists, Dr. Davis and team quickly and successfully repaired the duodenal obstruction and TEF at just one day old.

Home for the Holidays
Seamus spent much of his recovery time in the NICU, where the neonatal team managed his post-operative care. There, he began gastrotomy tube feeds and speech therapy and was cleared to go home ahead of the holidays on Dec. 15.
It was a difficult recovery that included some initial challenges with feeding and weight gain, but close collaboration between the parents and care team made all the difference.
“It’s a rocky road with lots of ups and downs,” said Dr. Davis. “It was really helpful to have parents that were steadfast and able to navigate the waves as they came, which made things so much easier because the communication was so good.”
Certainly, being able to receive coordinated, specialized care in one location was instrumental in both Liberty and Seamus’s recovery.
“She was able to be delivered at a hospital, have her baby stay at that hospital and then have the care coordinated between the neonatology unit, the pediatric surgeons and the cardiac intensive care unit without ever having to leave the hospital, sort of all in continuum,” said Dr. Schwendeman.
Now nine months old, Seamus is thriving. His heart defect was successfully repaired in May, and he is growing well and meeting developmental milestones. When he was discharged from the NICU, Seamus was in the third percentile for growth. As of his latest pediatrician visit, he is now in the 45th percentile. He recently started solid foods with ease and is a big fan of Oreo cookies and blackberries.
“Dr. Davis’s attention to detail and his bedside manner was phenomenal,” said Joshua. “It was a really hard recovery, and seeing Dr. Davis’s dedication to that was comforting to know that we had a great surgeon that was taking care of our kid.”

The Riggs’ share their story with NBC 5 Dallas-Fort Worth:
Learn more about our neonatology services, pediatric surgery services or find care in your area.